With most apraxic children it’s not that they physically ‘can’t’ blow bubbles or blow out candles etc. -it’s that they can’t do it when they want to/on command -a motor planning problem. Of course each child is different and in some cases children also have a weakness problem on top of the motor planning problem. This is why it takes a comprehensive evaluation by both medical and speech professionals. In addition, if a child is not responding to the therapies -it’s possible a misdiagnosis was made -and/or the child also has other undiagnosed underlying issues which are not being addressed as well. (another good reason for multisensory!)
There are also many activities parents can do at home with their child to promote the development of speech. These are detailed in the Guide for Parents from Contemporary Pediatrics written by Lisa Geng. Ms. Geng is co-author of The Late Talker What to Do If Your Child Isn’t Talking Yet. This guide was part of an article was originally published by “Contemporary Pediatrics” on November 1, 2004. You can read the article here.
Links with advice from my son Tanner’s awesome private preschool SLP Michelle A. Ortega, M.S., CCC-SLP
Feeding Strategies To Increase Sensory Organization
1. Increase the tactile input of the food by mixing textures. Add sliced fruit to yogurt and applesauce. Use milk sparingly on dry cereal to maintain crunchiness. Spread peanut butter on celery, or ranch dip on raw vegetables.
2. Avoid giving large pieces of food such as bagels or a hard roll. While the texture of these foods is good for chewing, children tend to sink their teeth in and rip off pieces rather than biting or chewing. Cut bagels, sandwiches, etc., into finger width strips for easier biting and chewing.
3. Increase the taste of foods with flavorings. You may experiment with spices not commonly used by children, such as pepper, Tabasco, mint or garlic.
4. Cut meats into small cubes to stimulate rotary chewing Cut raw vegetables into french-fry shaped strips.
5. Vary the temperatures of foods presented.. Freeze peas or cut up grapes for cold snacks. Serve warm (not hot) drinks through a straw. Prepare frozen fruit drinks and ask the child to identify flavor combinations.
6. Play food identification games. Cube some raw fruits and vegetables. Have the child close his/her eyes and place a cube in his/her mouth. Ask the child to identify the food by taste. Talk about texture, temperature and taste. You can also present warm cocoa/chocolate milk through a straw and ask the child to identify the temperature.
Strategies To Enhance Mealtime
1. Make a point to set a calm, relaxing tone for the mealtime. Control the lighting, sound and movement in the eating environment.
2. Establish “sitting behaviors”:
- Make sure the child is in a comfortable, well-supported seat.
- Have small fidget toys or books at the table to entice the child to sit.
- Make a placemat out of photos or pictures of favorite items and cover it with clear contact paper to give the child something for visual focus.
- Start with 5 minute increments (working up to 15 minutes)
- to encourage success. But… once the child leaves the table, mealtime is over.
3. Help the child establish regular hunger-satiation cycles by limiting eating to mealtimes and scheduled snacks. Contact your pediatrician to learn about appropriate serving sizes recommended for your child’s age. They are probably smaller than you think.
4. Discontinue all sip-cup use. Discourage your child from walking around with a juice cup in his/her hand. Drinks can by served in flip-top cups with internal straws, juice boxes, or sports bottles with straws on the go. Open cup drinking should be encouraged at all mealtimes.
5. Some children snack (chew) or drink (suck) for organizational, calming and arousing purposes. Replace the snacks with other positive oral behaviors.
Oral motor tips
- Increase frequency of tooth brushing.
- Toothbrush with an electric toothbrush.
- Allow oral exploration with hand-held massager.
- Oral motor toys (whistles, bubble blowers)
Here is a page of articles from. Each article below from TalkTools is a PDF If you are unable to open and would like me to cut and paste any or all of the following just let me know!
ARTICLES
- A Sensory-Motor Approach to Feeding, Lori Overland, M.S., CCC/SLP
- Targeted Treatment: Cranial Nerve Based Assessments, Alyssa Banotai featuring Jennifer Jones, PhD
- The Problem with Pacifiers, C. CLairborne Ray
- Red Flags of Children with Sensory-Motor Feeding / Speech Deficits, Emilia del Pino, M.S., CCC/SLP
- Sara Rosenfeld-Johnson’s Approach to Oral-Motor Feeding and Speech Therapy
- OPT as an Effective Tool in Aiding Non-verbal Children with Autism in their Utterance of Vowels /a/, /e/, /i/, /o/, /u/ and Consonants /b/, /m/, and /p/Saturnino, Sylvia Elizabeth C.
- Connections Between Tongue Placement and Dental Alignment
- The Effect of Lip Strengthening Exercises in Children and Adolescents With Myotonic Dystrophy Type 1
- Effective Exercises for a Short Frenum
- Efficacy of Using an Oral-Motor Approach to Remediate Distorted /r/
- Food for Thought
- Food Sensitivity in the Down syndrome Population
- Hard Facts to Swallow – Therapists working with feeding disorders
- Horns As Therapy Tools Part 1 and Part 2
- Moebius Article
- Mother Knows Best -Sippy Cups
- Oral-Motor Issue: Letter to the Editor
- Oral Habits: Why They Exist and How to Eliminate Them
- PROMPT Article
- The Role of the Jaw for Feeding and Speech
- Speech Therapy & Occupational Therapy: What’s the Connection? Oral-Motor, Sensory, and Feeding Skills
- Sippy Cup Article
- Straws as Therapy Tools
- The Oral-Motor Myths of Down syndrome
- Treatment of Children With Speech Oral Placement Disorders (OPDs): A Paradigm Emerges
- What’s Next? Blankie? The Beloved Sippy Cup Comes Under Attack
- Support For Cleft Related VPI/VPD
Oral Exploration: The Window to Their World Introduction to Infant Mouthing
Did you ever wonder why babies mouth so much? They are learning about their world! Babies experience the world through their mouths – their mouth is their primary learning tool. Through this a baby will experience size, shape, texture, taste, and temperature; and at the same time will be preparing their mouth for more complicated oral tasks involved with feeding and speech development. Babies also use oral play and exploration as a source of comfort and organization. Whether it is a newborn sucking a nipple or a teething six month- old biting a finger, oral experiences are relaxing and comforting. Babies begin to explore with their mouths even before they are born. Thumb sucking has been noted in utero as early as 16 weeks gestation. At birth the sensation in and around the mouth is the most highly developed. Most children are eager to suck and should enjoy oral and facial touches from caregivers, soft blankets and warm hands. By 4-6 months most babies have now developed greater body control and strength. They are learning to sit without support, reach for and hold toys, and bring toys to their mouths. Now the learning really begins! Everything must be taste-tested and explored, licked and drooled on! It is at this point where concerns about germs or choking are high. But don’t worry, as long as you keep a fairly clean house and monitor what objects are available, there should be no problem. Remember, keeping babies from mouthing and drooling on objects and toys will keep them from learning and being comforted.
Children with medical or developmental difficulties
Children with medical or developmental difficulties may lack these early oral experiences. Children with motor difficulties may not have the motor ability to hold toys or bring them to their mouths, and therefore have limited opportunities for oral exploration.
Children who have experienced hospital procedures such as intubation, suctioning, etc. can often develop the idea that the mouth and throat hurts and should be avoided. Similarly, children with reflux who experience discomfort during and after feeding may also associate oral experiences as painful and unpleasant. As parents and caregivers, we need to identify situations or difficulties that may interfere with a child’s abilities to experience their world through oral exploration. By providing pleasurable oral and facial input, oral development can begin to re-shape early learning experiences and set the stage for more positive and earlier experiences with food.
Some children who have not gone through the important oral motor exploration stage fully or at all go through it when they are started on nutritional strategies.
 My Child Can’t Drink From a Straw- Any Tips?!
My Child Can’t Drink From a Straw- Any Tips?!
There are therapies to help a child work on drinking from a straw and there are special cups and straws you can purchase to help. But perhaps there are things you can try first. My son Tanner had severe oral apraxia -so we had to work on drinking from a straw too. Even though there are other methods -here are the three key things I found to be awesome for tricking his body into drinking from a straw. (tricking – is a great word to put to use in regards to apraxia)
- Use the juice boxes and put the straw in -and squeeze the juice box so the juice goes up the straw to get him started. You can also do this by putting little straws into the puddings, apple sauce and kid yogurts they now have in tubes.
- Cut the straw really really short. All they need then is a tiny bit of suction and the liquid comes up. Gradually cut the straw less.
- Have your child dip the straw into the liquid and then put their finger over the top of the straw and lift the straw up out of the liquid. Their finger will keep the liquid from coming out -but have them let go and they’ll see the liquid come out. Help them do this and bring it to their mouth. Probably best to do with water or outside!
- It’s all motor planning if it’s apraxia. So once you get it into their motor memory (through repetition while they are having fun with it and not feeling forced -they’ll get it.) Once they get it -make it tougher and tougher by…getting them milkshakes and giving them that with thin straws. They’ll need to work to get the shake! Besides -once they can drink something as thick as a milkshake through a straw -drinking just about any other liquid is a cake walk.
Tips For Picky Eaters click here
Inability to Blow and Imitate / From Sara Rosenfeld-Johnson M.S., CCC-SLP who is on the advisory board for the Cherab Foundation
Lisa, The reason for the confusion as to who is best suited to work on these oral-motor activities (i.e., “lick lips, stick his tongue out, blow, suck through a straw, etc.”) is really based on the fact that both professions are interested in developing these skills.
The skills of blowing and sucking impact on feeding and speech development. The same muscles that are used in feeding are used in speech. Both professions therefore feel it is in their job description to work on the activities. Both are right. In our clinics we share the goals but use different techniques. The O.T.’s are generally interested in gaining function for independence while we SLP’s want not only function we want normal movement. Speech is superimposed on normal movement so when we talk about straw drinking we talk about it in a hierarchy of muscle development as in the TalkTools Straw Hierarchy. When we talk about blowing we create our programs to develop adequate airflow for extended speech statements. You need more air for a 5 word phrase than you do for a 2 word utterance. Therefore, instead of just picking up any horn or blowing cotton balls we again work in a hierarchy of abdominal grading activities (Horn Blowing Hierarchy or Bubble Blowing Hierarchy.) I am just thrilled that both professions are claiming the goals as their own. It was not so long ago that SLP’s did not see the benefit of working on non-speech movements for the development of speech clarity.
~Sara Rosenfeld-Johnson
Advice from Sara Rosenfeld-Johnson M.S., CCC-SLP advisor to CHERAB
“Hi Lisa, I am going to send you the program that I use for kids who cannot learn to blow. Remember that each child is unique and this is a generic approach. It must be tailored to each individuals needs. I have taken it from a Program Plan that I wrote for a child named ___. When you re-write it please omit the name.
I had a terrifc time at the conference. You should be very proud of all that you have accomplished! Sara Rosenfeld-Johnson
Pre-Hierarchy Horn/Volitional Exhalations: This technique will be most effective if it is used by an Occupational Therapists who understands how bouncing can stimulate oral exhalations. Teach ___ to blow the Pre-Hierarchy Horn using the following protocol:
a. Place ___ on the therapist’s lap as both sit on a large therapy ball. Work with her back facing your chest. Use the palm of your non-dominant hand to support her jaw. Bounce up and down on the therapy ball. Remain at this level until you are sure that she is comfortable with this play activity. As skills are mastered, progress to “b.”
b. Place ___ on the therapist’s lap on the therapy ball. Use the palm of your non-dominant hand to support her jaw in a slightly open-mouth posture. As you bounce onto the ball say a whispered “Hoo” sound. Use your other hand to press gently on her abdominal muscles. (Goal: To associate the sound of exhaled air with the escape of air from her mouth), 10 times. As skills are mastered, progress to “c.”
c. Place ___ on the therapist’s lap on the therapy ball. Use the palm of your non-dominant hand to support her jaw in a slightly open-mouth posture. As you bounce down place the palm of her hand in front of her mouth so that she will feel the exhaled airflow on her hand. Make sure to reward her verbally if you feel any exhaled air coming from her mouth. Continue to say “Hoo” in association with exhalations, 10 times or until a connection is made. As skills are mastered, progress to “d.”
d. Place ___ on the therapist’s lap on the therapy ball. Use the palm of your non-dominant hand to support her jaw in a slightly open-mouth posture and your fingers to give assisted lip rounding. As you bounce down on the ball place the Pre-hierarchy Horn in her mouth, close her lips around the horn and wait for the horn sound to be made. (Goal: To associate exhaled air with sound production), 10 times. As skills are mastered, progress to “e.”
e. Repeat this technique, bouncing with reduced force, until she is blowing the horn without any bouncing.
f. Once ___ makes the connection that she can blow the horn with her own volitionally controlled airflow you can eliminate the therapy ball from the activity. Transition the horn blowing activity to the therapy chair. Repeat 10 blows on the Pre-hierarchy Horn on the therapy chair before introducing Horn #1 on the Horn Blowing Hierarchy.
9. Horn Blowing Hierarchy: Do not introduce this technique until Myra is able to blow the Pre-Hierarchy Horn consistently in the therapy chair. Begin with Horn #1, requiring 5 blows of any sound duration each. Remember to remove the horn after each successful blow. Monitor to insure that she is not moving forward or elevating her shoulders as she blows the horn. The movement should be isolated to grading in the abdominal muscles. Once she achieves 25 blows on Horn #1, without any evidence of compensatory posturing, progress to Horn #2 on the hierarchy.* As you progress through the Horn Blowing Hierarchy, note that the sound duration will increase intermittently. (Goals: Abdominal grading and lip closure)”
~Sara Rosenfeld-Johnson
“Lisa, Please forgive me for not answering you sooner, I have just returned to Tucson after a very long lecture series and had a million (well almost) e-mails to answer. I have to say that I am very impressed by your answer to that mother Sandy. It is refreshing to read something from a parent that indicates that she/her understands what is involved in apraxia. So many professionals do not have a clue.”
Sara Rosenfeld-Johnson, M.S., CCC-SLP
Hi Sandy!
You always raise good points. I just want to add to your thoughts on something you may have missed.
With apraxia -the child has trouble motor planning movements to his tongue, lips, and jaw together properly -and typically also has trouble with breath control -possibly other aspects as well.
Apraxia doesn’t always start and end with the mouth -it can also be internal. With breath control -I’ve pointed out and (many) others have also reported the same -that apraxic children (even teenagers) -who obviously have no trouble at all breathing in and out of their noses all day and night -when “asked” to blow out of their nose into a tissue -will breathe ‘in’ instead!
Many apraxic children have to be taught to motor plan how to blow out of their nose ‘on command’ Sara has “nose horns” to address this motor planning problem -which obviously has nothing to do with dysarthria (or eating or feeding problems -the other problem known to be addressed with oral motor therapy). Proper breath control is crucial for speech.
It was also oral motor therapy that helped Tanner’s oral apraxia, helped stimulate the nerves in and around his mouth to teach him how to smile -or lick his lips. Those issues were not from weakness -he could do them -just not on command. Oral motor therapy also helped increase the sensory awareness to address his DSI. Oral motor therapy will of course help a child who has -or also has weakness – or dysarthria, or eating and feeding problems -however you don’t have to have low tone or eating or feeding problems to at least “try” oral motor therapy to address motor planning problems and sensory problems.
Keep an open mind -we are breaking new ground -so many things that we spot as parents will be in the literature years down the road – reported then as a “new” discovery. For now -we have to stick together and report what works for our child, whether it goes with or against the grain. There quite honestly has not been enough studies done yet to understand apraxia -what it is -why it’s on the rise -and what helps it best for anyone to assume anything yet.
We can hope that by sharing it as a group -we can figure out what will work for most -then the PhDs and MDs can do research to tell us “why” it works -so word will get out to the rest out there -to bring them a voice too. I believe again “multi-sensory” approaches are key for most of our speech and language impaired children -as has been found with most LD children. So don’t ever stop looking outside the box and limiting your child to only one approach. We will address this at the Apraxia Conference scheduled for May in South Carolina (information at the CHERAB website http://www.cherabfoundation.org (I’m sure that our advisor Sara Rosenfeld-Johnson, MS, CCC/SLP http://www.talktools.com/ will also reply when she has a chance!)
=====
Lisa Geng
President CHERAB Foundation
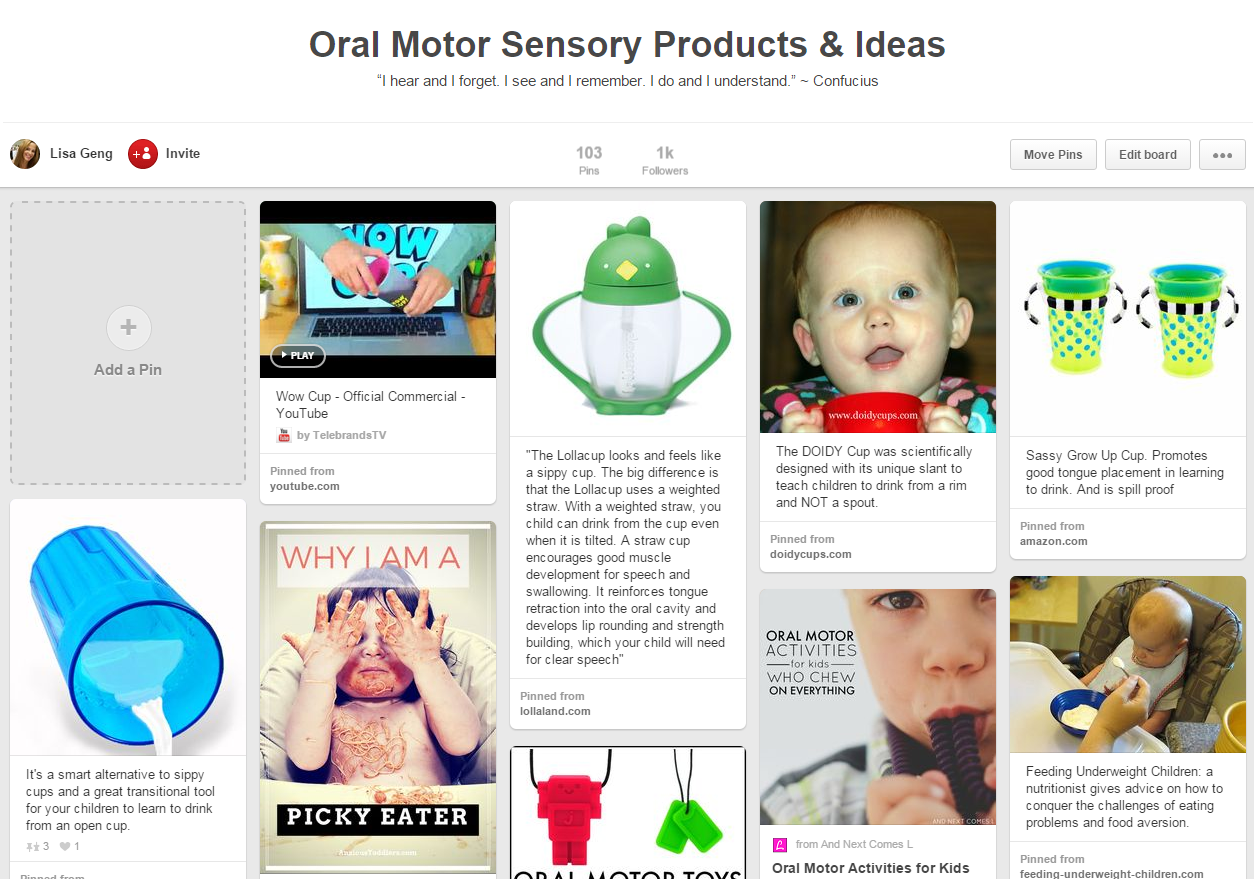
The Sippy Cup Issue
What a great email I got today! An SLP forwarded me a link to an article on why “sippy cups” are not the best choice for transitioning kids off of bottles. In this article in Baby Talk they talk about the fact that to drink from a “sippy cup” the child has to use a suckle pattern. The best quote is from an SLP “There are only a few sounds we produce with the tongue out like ‘th.’ Most words are spoken with the tongue in, and the sippy cup does not encourage that.” Finally! I have been teaching this same information in my class, A Three-Part Treatment Plan for Oral-Motor Therapy, since 1992 but for some reason the message has not gotten out there. Even though Jonathan Eig wrote an article many years ago in the Wall Street Journal, in which I was quoted, this is the first resurface of the issue I’ve seen and I’m elated.
I have spoken with many dentists who also discourage the use of these cups as they foster an open bite. These cups are carried around and allow kids to have a sugared liquid in the mouth frequently throughout the day. For this reason the incidences of cavities is increased in kids who use them habitually. Many pediatricians don’t like them because a child can drink from them with the head tilted back allowing liquid to enter the Eustacian Tubes so these kids are at greater risk for ear infections.
There are so many reasons why they should not be used especially with our clients with tongue-thrusts which already impact negatively on their speech and feeding skill development. Using a recessed lid cup, Honey Bear with Straw or a Straw Drinking Hierarchy (admittedly biased source – other sources exist but I cannot vouch for quality) is a much better way to ensure adequate liquid nutrition, avoid spilling and actually improving oral placement and movements for speech
Sippy Cut Alternatives
Find many alternatives on Pinterest- click below for a few (no vested interest in any particular brand. Also can’t recommend one over the other but a number of them are apparently recommended by doctors or SLPs)
Gum Chewing as Oral Motor Therapy
“As an SLP who works with kids apraxia, autism, & eating challenges, there are many therapeutic uses of chewing gum. It provides deep proprioceptive input into the jaw, so it can be very organizing for kids. When introducing gum, it’s important to teach the child HOW to chew it. Depending on the age & skill of the child, he/she may not know how to chew gum in an organized manner. Talk Tools has a great gum hierarchy that I use to teach this skill. If a child is not organized in the chewing, then it’s not going to provide optimum input. Many kids have difficulty with the components of gum chewing: tongue lateralization, bolus control, saliva control, graded & coordinated jaw movements & lip closure.
Jaw skills should always precede lip, & then tongue. There are other structured oral exercises also which may need to be taught first or in conjunction with gum chewing. So ask your SLP if your child has all of the skills needed for gum chewing. It’s harder than it looks!
I forgot to add info about taste & texture! I recommend gum w/ sugar when a child can’t chew for very long but w/o sugar–b/c it gets harder over time–when he/she will chew for a while. If a child has low tone, I usually try a high taste/flavor like cinnamon, lemon, etc.
I usually start with one half of a piece of gum & increase to a full piece once they are chewing independently. Rarely do I use more than 1 piece at a time. This may be indicated for older kids who are independent, for purely sensory input
Warmest wishes,
Barbara A Taylor, M.S.,CCC-SLP
CEO, Help Me Speak, LLC
www.helpmespeak.com
Parent Tip For Drooling
By Lisa Geng
When you look at your child and he is drooling, take your finger and run it down your throat and say “swallow” to remind him to swallow. After awhile, you do not need to say “swallow” you will only have to run your finger down your throat as a sign for him to remind them to swallow. This way it doesn’t draw attention to him and embarrass him in public situations. (Teachers can do it too, etc.)
Drooling could be a sign of an oral motor problem -typically it’s a sign of weakness, typically not a sign of a motor planning disorder (even though some children with the motor planning disorder apraxia will drool because it’s not unusual for motor planning and weakness problems to co-exist)
There is an Drooling Remediation Kit from Talk Tools
And more information on drooling from the Miami Children’s Brain Institute:
Sialorrhea is the medical term for drooling (also known as ptyalism), and refers to the flow of saliva outside the mouth.
Read more
Classification
Drooling may be caused by:
- excess production of saliva
- inability to retain saliva within the mouth
- problems with swallowing
Common causes
Isolated drooling in infants and toddlers is normal and is unlikely to be a sign of either disease or complications. It may become worse when the child is teething. Drooling in infants and young children may be exacerbated by upper respiratory infections and nasal allergies.
Drooling also is common in children with neurological disorders or developmental delay. In these children, the reason for excessive drooling seems to be related to:
- lack of awareness of the saliva in the mouth
- difficulty swallowing
- weakness of the lips, tongue, or jaw
Drooling associated with fever or trouble swallowing may be a sign of a more serious infection.
A sudden onset of drooling may indicate intoxication, either accidental (such as by pesticides or envenomation) or deliberate (such as alcohol).
Home care
Care for drooling due to teething includes good oral hygiene. Popsicles or frozen bagles may be helpful. Care must be taken to avoid choking when a child uses any of these objects.
Treatment
Treatment is most effective when the underlying problem is identified and targeted. Possible treatments include:
- Speech therapy
- exercises to increase awareness of the mouth
- training to increase frequency of swallowing
- swallowing practice with a speech therapist
- Good oral hygiene
My son Tanner was diagnosed with both oral as well as verbal apraxia
Not all children with verbal apraxia will have oral apraxia, but it’s pretty much a given that all children with oral apraxia will have verbal apraxia. Before Tanner learned how to smile he didn’t even try much and most times just had a blank look on his face as you’ll see in the photo below.
Tanner didn’t move his face much. He typically would just stare at you without any smiles. We called him the “serious baby” at this point not knowing he had classic signs of oral apraxia. Tanner couldn’t even lick his lips! If Tanner had peanut butter or chocolate on his lip he couldn’t even lift his tongue to try to lick it off. Tanner would use his fingers to push the food on his lips into his mouth. Also, Tanner couldn’t blow the candles out on his second birthday cake. In fact, he couldn’t blow bubbles until almost 3 years old even though he tried and tried. Nobody, including Tanner’s Pediatrician, or his first Speech and Language Pathologist, knew these were all strong warning signs of Oral Apraxia, which can occur with Verbal Apraxia. There are professionals who are knowledgeable, you just have to find them.
Tanner was able to smile once in awhile, and when he did, he lit up the room.
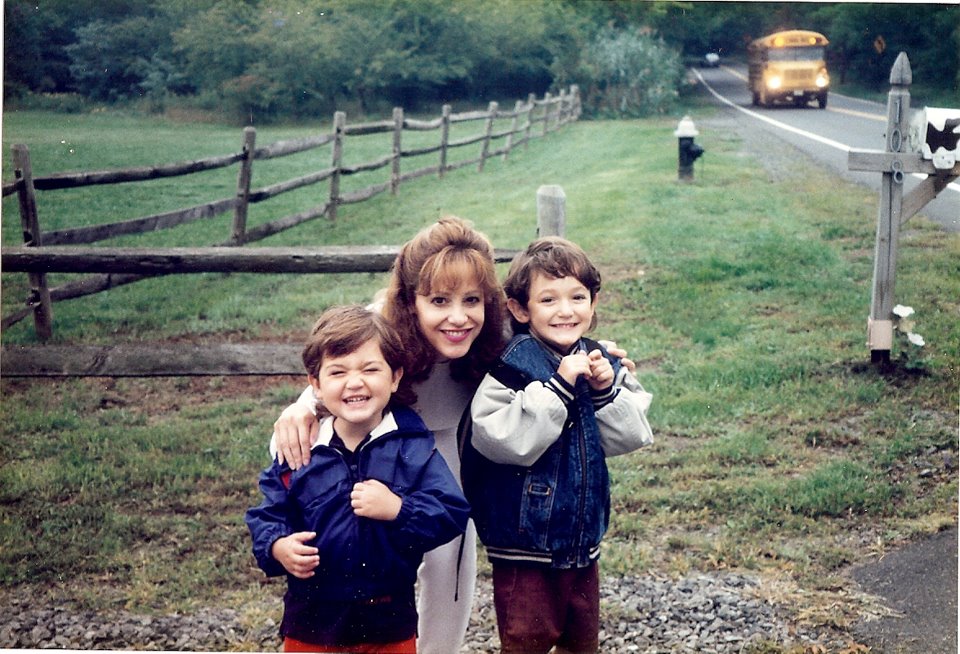
Below is me with my sons Tanner on the left, and his brother Dakota on the right on their first day of school. Preschool for Tanner, kindergarten for Dakota. We were all so excited, and you can see the school bus in the background. Tanner had to learn how to smile due to his oral apraxia. When Tanner was learning to smile he would smile and close his eyes. We’d then say “Tanner open your eyes” and he’d open his eyes and open his mouth. Then we’d say “Smile again” and again he’d smile and scrunch his face like in this photo again which was his classic smile for awhile.
Tanner’s background is here which is a letter I wrote to parents years ago to raise awareness about oral and verbal apraxia. But most don’t know what oral apraxia is or how it can affect a child and his family. The impact it can have in school when that “blank look” is taken by the teacher as not understanding. Tanner’s oral apraxia affected him for most of his life up till recently. At age 11 after years of therapy his one speech therapist Dr. Renai Jonas CCC-SLP who I highly respect, even tried hooking electrodes to his face to stimulate the nerves with little help. Tanner responded to nutrition too somehow which is remarkable after the years of therapy. We are so thankful! Here is Tanner today.
Signs of Oral Motor Dysfunction
|
Possible Oral Apraxia or Oral Motor Warning Signs from the Cherab Foundation There are two types of oral motor problems. Oral Apraxia is a disorder where the child, who typically is a “late talker” is unable to coordinate and/or initiate movement of their jaw, lips and tongue (articulators) on command. An Oral Motor Disorder, which could be a different oral motor problem than apraxia (could be from weakness/dysarthria for example) is the second type, in which the child is unable to coordinate and/or initiate movement of normal eating movements (vegetative activities.) Here are some possible warning signs of the two types of oral motor problems, written by Lisa Geng, the parent of two children who were diagnosed by a neurologist (Trever. DeSouza MD) and a neurodevelopmental pediatrician (Marilyn Agin MD) with two different types of oral motor problems, with help from Cherab’s advisor, Sara R. Johnson, CCC/SLP. Can your child do the following regularly or on command:
If your child cannot do all or some of the above, this may be a sign of Oral Apraxia, which is worth looking into with medical and speech professionals. Or does your child…
If your child does all or some of the above, this may be a sign of Oral Motor problems, which is worth exploring with medical and speech professionals. If you are seeing any of the above signs, seek out the services of a Speech Language Therapist for an evaluation of these skills. This can be done through your State’s Early Intervention Programs, a free federally funded program for qualified children from birth to three years of age or through your school district’s preschool disabled program, a free program for qualified children between the ages of three to 6 years. You can also contact the American Speech Language-Hearing Association in Rockville, Maryland for a list of certified clinicians in your area. It is very important to have an ACCURATE assessment completed by a skilled clinician. You may also want an evaluation from a developmental pediatrician, or pediatric neurologist to look for signs of low tone (hypotonia). |
A Reason to Know the Signs of Oral Apraxia
I just received an email from a parent who has a child that is about 18 months old, is nonverbal, and was recently diagnosed with oral apraxia. She stated that she was a “blubbering idiot” because she cried, and I sent her this response, which may help some of you as well. ‘The Moment I Realized My Son Was Special Needs”
We didn’t ask for this when we decided to be parents; this is an added surprise. It doesn’t mean that it’s bad, it’s just not what most people go through.
Believe me I know what it’s like to go from “he’s just a late talker, but man this kid is SO smart, just look at him!” and believing he is completely normal, to finding out a day later that…
He is not talking because has a severe neurologically based speech disorder which is called all different names which can mean different things to different people since the medical and speech professionals and the world can’t agree on just one name so it’s called apraxia or dyspraxia or oral or verbal apraxia or oral motor disorder or motor planning disorder or phonological motor planning disorder but no matter which name you call it most of the world is still ignorant to it but if I don’t find out what he needs for appropriate therapy through insurance and school when it comes to speech and occupational and physical therapy as well as appropriate ways to educate him he may never learn to talk, and in addition he always had “soft” neurological signs like hypotonia and sensory integration that up until yesterday I didn’t even know existed and nobody not even his pediatrician ever knew he had and it took a neurologist and a developmental pediatrician to point these “soft” neurological signs out to us.
Sure there are warning signs of oral apraxia, which can be spotted long before verbal apraxia. Problem is that most people don’t know what they are. Below are a few of the signs of oral apraxia that our son Tanner displayed. Not every child with verbal apraxia has oral apraxia as well, but it is not uncommon. Outside of the obvious, the reason we believe that we need to include this page in this website is because parents have read about oral apraxia at this website and then, based upon the “signs” of oral apraxia they learned about, they took their 2 year old child for an evaluation, where the child was diagnosed with oral apraxia by a professional.
We have been told that besides the Cherab Foundation websites, there is nothing else on the internet with Parent Friendly Signs Of Oral Apraxia. (note this was written just a few years ago. Since then others are now sharing more)
Reason for more awareness for oral apraxia
When my son Tanner’s neurodevelopmental pediatrician, a Medical Director for Early Intervention in New York, saw Tanner for the first time at 3 years old, she shook her head and said, “I could have told you a year ago this child had severe oral apraxia. He doesn’t know where his tongue is in his mouth!” She diagnosed Tanner with apraxia after a brief examination. The apraxia was never seen by Tanner’s pediatrician, and it took months for even a speech therapist to diagnose Tanner with apraxia! Tanner could have received appropriate therapy a year earlier if we had only known.”
- If there is not information out there that can be understood by people outside the field of speech, then there should be, for important reasons.
- Experts state that oral apraxia can be diagnosed as early as 18 months, which is over a year younger than a positive diagnosis of verbal apraxia is usually received.
- For early intervention, “the sooner the better” for apraxia. Awareness should be raised about oral apraxia while we continue to raise awareness about verbal apraxia.
- Oral apraxia appears to be a red flag to verbal apraxia A diagnosis of oral apraxia is almost definitely means a diagnosis of verbal apraxia. Since oral apraxia can be diagnosed as young as 18 months, we can provide our apraxic children the best possible chance for appropriate early intervention.



http://www.sandiego6.com/news/local/Autistic-Abuse-Case-Suspects-Plead-Not-Guilty-170802936.html What a shame these parents have so many positive supports in place and these caregivers chose to ignore these and abuse the patient. Just shocking stuff. Shows how abusive caregivers can’t undermine a parent’s effort in helping their autistic child. One caregiver is seen in videos released on news, shoving, kicking and punching this autistic young man because he’s forcing him to stay in room and in bed all day instead of walking him outside which is apparently his normal routine in day.
It’s really a nice and helpful piece of info. I am glad that you simply shared this useful information with us. Please keep us up to date like this. Thank you for sharing.
This video gave me some great information to help me work with a child in our classroom (4 year old – low parent involvement when younger) with symptoms of what you’ve described: tongue thrust, eating concerns, afraid to try foods or saying “I’m not hungry”. His teeth are widely spaced, he drinks milk with an open mouth, etc. Although I have an extended support system – to refer him for an IEP, I want him to “want to come to the meal table.” When I ask him “what do you like to eat?” he says “cake” . He comes to the meal table when I have “goldfish crackers and milk” 🙂 and when he brings a book that have movable parts. Thank you for your time
My 8 year old was diagnosed with late bloomers autism wen he was three and he has ADD and A DVD He does talk ,read or write. He can just say a few words like moma, daddy ,papa ,Nana and bubba. He goes to occupational therapy we’d be peach twice a week. He doesn’t like to brush so teeth. He grinds his the all the time He gets choke easly.He don’t know how to such on a suckered he bites it til gon He knows hat you are saying but he just can’t talk.
Hi Kimberly, you’ll want to know for sure if it’s autism or a developmental lag in speech/or impairment of speech with senstory processing disorder. For sure sounds like he has sensory processing disorder which in itself is not autism. The fact he’s already saying a few words, reading and writing at 3 is awesome! Does he currently have an IEP? Where would you say he fell on this matrix? https://pursuitofresearch.org/2013/03/22/speech-therapy-matrix/ There are a number of links for advocacy under that
When you wrote he has “ADD and A DVD” Did you mean to say ADHD -most just use ADD and ADHD interchangeably. I personally find it irresponsible on the part of doctors to diagnose any child before school age with ADHD or ADD -they are kids! Then they stick them on drugs which can potentially be dangerous and far more detrimental than a hyperactive 3 year old. You may want to read this page here https://pursuitofresearch.org/2013/03/15/diet-may-help-adhd-more-than-drugs/ Even at 6 years old (school age) if the activity is not interfering with school or social I wouldn’t even consider the diagnosis -too many kids are misdiagnosed with it…when they are just kids. In addition if he does have a speech delay or disorder he may be frustrated in his lack of ability to communicate which can create some negative behaviors. I’d find another doctor…actually what type of professional diagnosed ADD in your 3 year old? I was even annoyed the AAP now allows diagnosis as young as 4 -but don’t even believe anyone is able to diagnose a 3 year old with ADD.
You may want to get my book The Late Talker as there are many strategies in there to help. About the feeding issues -choking -that is something that is easily covered by insurance as it’s a medical condition. You’ll want to seek an oral motor speech therapist -this page may help too https://pursuitofresearch.org/2012/07/22/oral-motor-dysfunction-exercises-and-therapy-for-autism-and-apraxia/
I had the hardest time finding an SLP who was trained in oral motor therapy. My son didn’t have trouble eating but he had trouble with many of the other things you have mentioned here and it was frustrating that many of the therapists I brought him to didn’t believe he required oral motor therapy. I finally found an SLP who combined traditional and oral motor therapy in her approach and it made a world of difference in my son’s speech.
Hi Lisa,
This is such a great post and so well documented! I was wondering if you would like to write another one these days, using more recent research about TalkTools. Let me know if this could be of interest to you. Thanks!
Sara has been an adviser to the nonprofit Cherab Foundation for over a decade now. I would love and appreciate more recent research on TalkTools Will send you a direct email. Thank you!
Lisa Geng
President CHERAB Foundation
Communication Help, Education, Research, Apraxia Base
Conceptualist for IQed “Approved for the Feingold Diet”
“Help give our cherubs a smile and a voice”
When my son was born, I was not told half the information your are giving. My son has been in Speech Therapy about a month after being born; due to having a Laryngeal Cleft in his throat. He has had three surgeries up to 2008 to repair it. Then around 2009 they gave him the okay to eat by mouth; that it was safe to do so. When he was around seven in 2014, he still wasn’t talking or eating. Then I started getting excuses from therapists stating why they were not able to help him much or why they couldn’t take him in; silly excuses. It became so tiring that I took it upon myself to do his Speech Therapy. He is now nine going on ten in May this year 2017, and no actual words or eating; but he tries. So, I’m going to give some of things you suggested and see what happens.
Jennifer I know how frustrating it can be for us as parents to at times learn more online than from our child’s professional, on that other hand that is the beauty of the internet. Most of us tend to look at all speech therapy as the same, and all SLPs as the same, but that’s not the case. There are so many types of speech therapy, and as I always point out not every professional graduates at the top of the class. Most SLPs are good, but there are some that are above or below average. If you are seeking private therapy you can seek the best- which sometimes means traveling a bit further than your home. I highly recommend parent recommendations if you can secure some.
I also wanted to share this page with you https://pursuitofresearch.org/2016/07/26/vpd-support/ based on what your child has gone though -there is a support group linked to on that page that you may want to join. I hope this helps -just remember it’s never too late. There is always hope!
Lisa Geng
President CHERAB Foundation
Communication Help, Education, Research, Apraxia Base
Conceptualist for IQed “Approved for the Feingold Diet”
772-335-5135
“Help give our cherubs a smile and a voice”
Hi,what tools would help children with oral apraxia?
Hi Karen,
On the page you were on I had some of the recommended tools, but if you have an SLP that specializes in oral motor therapy they probably will recommend some. Oral apraxia is tough because it’s not a weakness, it’s a motor planning impairment. Did you see this page? https://pursuitofresearch.org/2017/02/03/why-more-should-know-what-oral-apraxia-is/
To be honest when it came to oral apraxia that was harder to overcome than the verbal as I don’t believe as many kids have it and don’t believe all SLPs know how to address it. As these conditions are on the rise you may be fortionate in finding an SLP who has knowledge in working on a child with oral as well as verbal apraxia (because if there is oral apraxia, you can pretty much guarantee there is verbal as well)
Have you also had your child to either a pediatric neurologist or developmental pediatrician to confirm or rule out soft signs? https://pursuitofresearch.org/2014/07/29/parent-friendly-soft-signs/
Best,
Lisa
Lisa Geng
President CHERAB Foundation
Communication Help, Education, Research, Apraxia Base
Conceptualist for IQed “Approved for the Feingold Diet”
772-335-5135
“Help give our cherubs a smile and a voice”