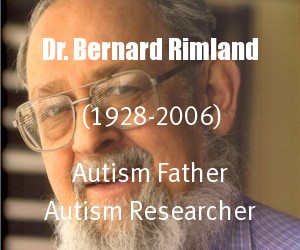
“Your child doesn’t have PDD. There is no such thing as PDD. Your child may be autistic, or have a condition like autism, or many characteristics of autism, but he doesn’t have PDD because there is no such thing. PDD is a label concocted by psychiatrists to cover up the fact that they don’t know what your child does have.” ~ Bernard Rimland, Ph.D. Autism Research Institute
For sure you want to know if it is or isn’t autism so you can secure appropriate therapies and placement. The diagnosis of autism (which is what is assumed today if a child has a diagnosis of PDD or PDD NOS) will most likely lead to therapies and placement that are appropriate for autism.
There are other diagnosis that may be more appropriate for the child to secure appropriate therapy and placement for the best prognosis. For example, due to apraxia or dyspraxia also being multifaceted communication impairments, most apraxic/dyspraxic children could fall into the PDD or PDD NOS diagnosis depending upon where they are diagnosed. When this happens however instead of a focus on speech and motor planning therapies, along with if needed sensory and strengthening therapies, all of which could be appropriate for an individual with apraxia or dyspraxia, the focus would most likely be more on behavioral therapies such as ABA. However ABA therapy which is typically appropriate for autism, is highly inappropriate and can even be detrimental if used to address the motor planning deficits of an apraxic or dyspraxic child.
For this reason, please don’t accept PDD or PDD NOS unless you are sure it’s autism, and if your child has mild autism, just say it’s mild autism. So I agree 100% with Dr. Rimland. Here’s one of my favorite articles on this by him: Bernard Rimland, Ph.D.
Plain Talk about PDD and the Diagnosis of Autism
Plain Talk about PDD and the Diagnosis of Autism
Written by Bernard Rimland, Ph.D. Autism Research Institute
Autism Research Review International, 1993, Vol. 7, No. 2,
Let’s start with the obvious: the label PDD (Pervasive Developmental Disorder) is a poorly understood, uninformative, confusing, disliked, and should be abandoned. The sooner the better. In fact, it should never have been adopted in the first place.
Over the years I have talked and corresponded with thousands of parents who have told me their child “has PDD.” I often respond by saying something like, “Your child doesn’t have PDD. There is no such thing as PDD. Your child may be autistic, or have a condition like autism, or many characteristics of autism, but he doesn’t have PDD because there is no such thing. PDD is a label concocted by psychiatrists to cover up the fact that they don’t know what your child does have.”
If any parents have been distressed by this blunt, unexpected harangue on my part, I would be surprised. The vast majority seem relieved to at last hearsomeone giving them straight talk about PDD. Parents live with their child 24 hours a day, 7 days a week. These parents realize that their handicapped child will in all likelihood be the central focus of their lives for the rest of their lives. They want to know the truth, insofar as the truth is known. They don’t want to be misled or misinformed by sugar-coated verbiage masquerading as informed fact. If we don’t know the right label for their child, let’s tell them that up front, rather than hide our ignorance behind the mystique of a pseudo-scientific label, presuming knowledge we don’t have, like PDD.
I am very much aware that creating suitable names for “psychiatric” or “behavioral” disorders is a difficult and thankless task. Look at what we have now: Schizophrenia is Greek for “split mind.” Mental retardation is a euphemism for low intelligence. Hyperactivity merely describes what everyone knows too well–the person is too active. Autistic means “day dreaming.”
Until we know what causes these things we are stuck with using a somewhat descriptive term to characterize them. I’ll agree to that, as a matter of necessity, but where does PDD come in?
The passage of time has led to widespread usage of the terms, schizophrenia, mental retardation and autism. There is little or no likelihood that PDD will be afforded similar acceptance.
In the Autism Research Review International (ARRI) (1991, Vol. 5, No. 2), we summarized an excellent statement, signed by 16 prominent European and U.S. professionals in the field of autism, titled “Autism is not necessarily a pervasive developmental disorder.” The authors noted that although the term PDD was introduced well over a decade ago, it has not really caught on, and is unfamiliar not only to lay people, but to the politicians and administrators, most of whom–thanks probably to Rain Man–are aware of autism. The article observes that the term “pervasive” is particularly inappropriate, since severely retarded persons, many of whom have chromosomal defects which affect every cell in their bodies. Autism, they point out, rather than being a pervasive disorder, is in fact a specific one, characterized by deficits in social and cognitive functioning.
Quite apart from the misleading and inappropriate semantics of the term PDD is a practical matter: autistic children and adults unfortunate enough to have the PDD affixed to them have often been–and continue to be–excluded from programs and services designated for those with autism, and which would benefit them.
Clearly, the PDD designation, along with its cumbersome bureaucratic baggage (i.e., PDD-NOS: “Not Otherwise Specified”) should be relegated to the Archives of Failed Attempts, where it will have plenty of company, while we go on about our business.
There are many more children with autistic-like disorders than there are children with autism itself. When I founded the Autism Society of America in 1965, I urged, and my recommendation was followed for many years, that all ASA stationery, brochures, and other printed materials carry the wording “Dedicated to the welfare of all children (later ‘children and adults’) with severe disorders of communication and behavior.” The need for an encompassing title for this group was evident even then.
Of the various labels that have been suggested, the one I like best is “autistic spectrum disorder,” which, I believe, was first suggested by Wing and Gould in 1979. The advantages of this term are obvious. For one, it acknowledges that there is a range of problems and of subtypes, and it does not pretentiously claim to be based on knowledge that is not yet available to us.
At the Autism Research Institute we have been working for over a quarter of a century on the development of more objective scientific means of diagnosing children with autism and related disorders.When my book Infantile Autism was published in 1964, it contained, as an appendix, a checklist designated “Form E-1” (E for experimental). Within a year E-1 was replaced by the Form E-2. As of June 1993, the Autism Research Institute has collected over 16,800 E-2 forms, completed by parents of autistic and possibly-autistic children in over 50 countries. (Form E-2 is available in eight languages.)Form E-2 is designed for completion by the child’s parents, and asks questions about the child’s early development and about language and behavior through age five an a half. (After age five an a half, autistic children begin to change in many ways, so it is better to rely on behavior prior to that age.) Once we receive a completed E-2 form from a parent or professional, we enter the data into our computer, derive a score which tells the child’s position to the continuum ranging from “classical autistic” at one end to “not autistic” on the other, and mail a report to the sender. We have performed this service, free of charge, for well over a quarter of a century for thousands of parents and professionals world-wide. (Readers of the ARRI are invited to request E-2 forms and avail themselves of this free service.)A major purpose of this effort is to collect data for statistical analysis. There is no doubt that the “spectrum of autistic disorders” contains numerous subtypes, some of which are large enough to be identified by as our database of almost 17,000 E-2 Forms. We are already aware of some of these types, such as classical–Kanner’s Syndrome–autism, fragile X autism, Rett syndrome, and candida-caused autism. My colleague, Dr. Stephen Edelson and I are conducting factor analyses and cluster analyses of the E-2 database, in order to identify and characterize these and other subtypes. The database is large enough so that subtypes identified by cluster analysis within one segment of the database can be confirmed by cross-validation on E-2 data which was not used in the original identification of subtypes.
As this work advances we will report on progress in the ARRI, and in other places. Subtypes identified through this means of statistical analysis can be validated in a number of ways, independent of the E-2 database, including family history variables, clinical laboratory tests, and differential responses to drugs and other treatments. It is thus hoped to place the diagnosis–as well as the treatment–of “autistic” children and adults on a more scientific basis. I believe that progress in this field will proceed faster if we rely on the identification of subgroups through the analysis of statistical data, rather than on constructs based on speculation, conjecture, surmise and subjective impressions.
In the meantime, let’s get rid of “PDD!”
This article appeared in the Autism Research Review International, Vol. 7 (2), 1993. The Autism Research Review International is a quarterly newsletter published by the Autism Research Institute (4182 Adams Avenue, San Diego, CA 92116, U.S.A.).
LISA GENG