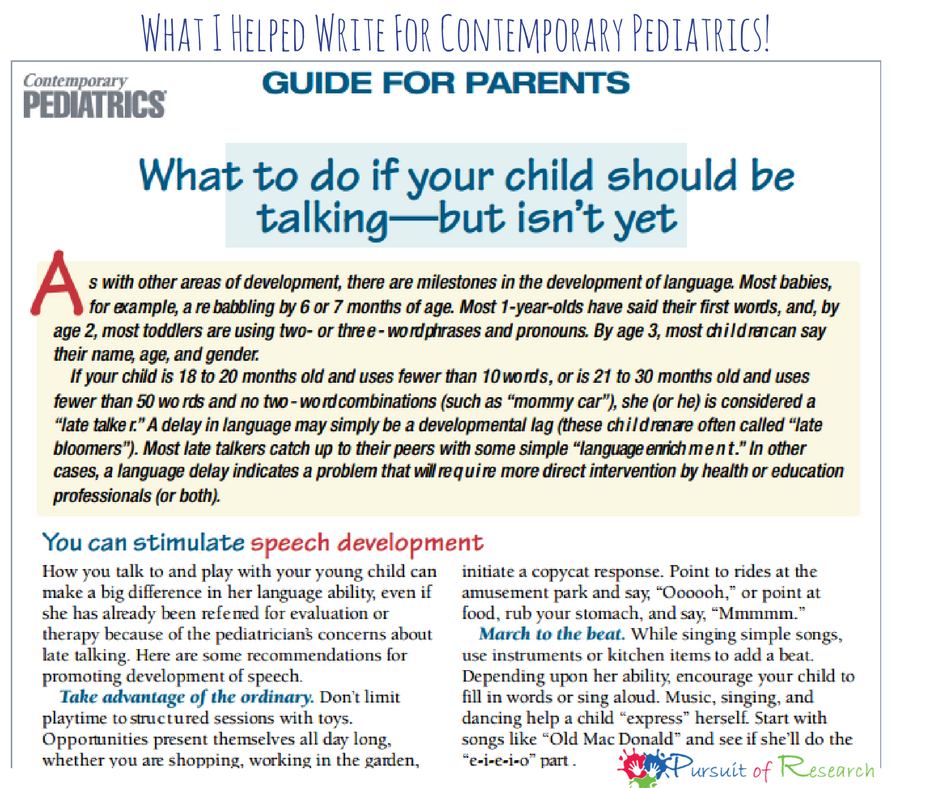
After The Late Talker book was published, as a mom was pretty excited when we were asked to write this feature cover article for “Contemporary Pediatrics” which is the trade magazine for hundreds of thousands of pediatric medical professionals nationwide! My one coauthor is a neurodevelopmental pediatrician and I was credited for the “guide for parents” The article below was published on November 1, 2004
The “late talker”—when silence isn’t golden
Not all children with delayed speech are “little Einsteins” or garden variety “late bloomers.” Some have a speech-language disorder that will persist unless warning signs are recognized and intervention comes early. Includes a Guide for Parents.
Contemporary Pediatrics Publish date: Nov 1, 2004
It’s been a busy day at the office, and you’re finishing up your last appointment—a 21-month-old with bilateral otitis media and fever. As you’re writing a prescription, the mother remarks, “Should I be concerned, Doctor? Joey hasn’t said any words yet. We believe he hears, because he goes running to the door as it opens when my husband comes in, and he becomes alert when I approach his room.” You ask whether Joey responds to his name and is able to follow simple directions. “Yes,” the mother answers, “but is it normal for a child to be so quiet? Joey did not babble much as a baby and has never said mama or dada. He just points and says ‘uh-uh’ or takes me by the hand trying to show what he wants. Lately, he’s become so frustrated when he can’t make himself understood that he throws himself on the floor in a rage.” She goes on to tell you that her husband is unconcerned because he heard that boys often speak late, and that the grandparents have told her that Joey just needs time. “They say Uncle Jerry didn’t speak until he was 3, and now he’s an accountant, and Aunt Mary spoke late and now she doesn’t shut up!”
What advice do you give this mother? Joey seems to be developing normally in every other way—he’s had a few ear infections before this one, all of which resolved without a prolonged period of effusion. But his delay in talking does warrant further assessment, and you decide to send him for a hearing test after his infection clears. Meanwhile, you tell the mother not to worry—boys often speak later than girls, and there seems to be a history of late talkers in this family. You let her know that if results of the hearing test are normal, you will follow up at the 2-year well visit.
Joey thus joins the ranks of “late talkers,” a term used to describe children 18 to 20 months old who have  fewer than 10 words, or those 21 to 30 months old who have fewer than 50 words and no two-word combinations. Typically, these children have no other problems. (For a glossary of terms pertaining to late talkers, see the box .)
fewer than 10 words, or those 21 to 30 months old who have fewer than 50 words and no two-word combinations. Typically, these children have no other problems. (For a glossary of terms pertaining to late talkers, see the box .)
Along with the newsworthy rise in the number of children in whom autism has been diagnosed are reports of an approximate 30-fold increase in the number of children with speech or language impairments since 1989, according to a 2001 US Department of Education (DOE) report.1 Those statistics show 7,801 cases of speech or language impairment among children born in 1983 (who turned 6 in 1989). Among children born in 1994, that number jumped to 211,984.1 This rise does not appear to be attributable to increased awareness alone, as there has been no comparable rise in other developmental disabilities (e.g., autism, four-fold increase; mental retardation, two-fold increase). The etiology of speech and language impairments is not completely clear, but a multifactorial etiology has been entertained (environmental factors; genetics; prematurity, i.e., increased number of low birth weight infants).
Speech and language delays are the leading developmental concern in parents of children younger than 5 years. Glascoe reported that when a parent had a single developmental concern, 65% of the time it was about expressive language skills.2In addition, according to data from the New York State Early Intervention Program (EIP), most referrals into the program are related to parental concerns about a speech or language delay. The largest number of children eligible for EIP (81%) are eligible because of problems in the communication domain.3
An estimated 15% to 25% of young children have some type of communication disorder.4 Language impairments are well known to accompany hearing loss as well as structural or oral motor deficits affecting the speech musculature, and they have been associated with autism, fragile X, Down syndrome, and a multitude of other syndromes. But even when these causes of language impairment are accounted for, there remains a large number of children who, for unknown reasons, experience difficulty developing speech and language.5
Although most late talkers do, eventually, catch up and speak normally, it’s important to be aware of warning signs that may indicate a communication disorder rather than a benign delay. In such cases, as with all communication impairments, early diagnosis and treatment are critical. And, even in cases of a child who is merely a “late bloomer,” there are steps that can be taken to promote the development of speech.
Predictors of continued language delay
You are certainly familiar with the unfolding of developmental milestones (Table 1,) and the variability that may be seen in a typically developing young child. That variability can make it difficult to tell if a patient has an innocent delay or something more serious (Table 2,). So, how can you tell if your young patient is just a late bloomer or has a speech or language disorder? And why not let nature run its course rather than have the child and family undergo an evaluation and possible interventions?
There are warning signs of a speech disorder that appear in the first years of life6 and that, if ignored, portend persistent speech problems. One major review in the speech pathology literature paints a profile of toddlers 18 to 24 months old who are at risk of persistence of language impairment at 36 to 48 months and who should receive early intervention.6 The greater the number of warning signs a child exhibits (especially the closer he gets to 3 years of age), the greater the need for early assessment. Those signs include:
- little sound play or babbling as an infant, with limited number of consonant sounds and, possibly, vowel distortion as a toddler
- poor verbal imitation skills; reliance on direct model and prompting
- immature play skills; little pretend play
- interactions with adults more than peers
- few communicative gestures (the late bloomer who caught up with his peers within a year used significantly more gestures than the child who had persistent delay)
- impaired social skills or behavior problems
- small vocabulary for age; less diverse verb repertoires
- comprehension delay of six months or greater relative to chronologic age
Moreover, several risk factors were found to impair speech and language development:
Family history, such as a strong heritability factor. There’s a higher risk of continued delay if one of a toddler’s parents or siblings had long-term language and learning difficulties.
Otitis media with effusion causing a fluctuating hearing loss during the period of speech development.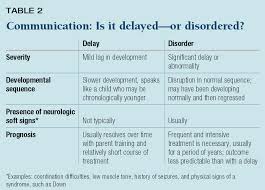
Low socioeconomic status and educational level. These families are more likely to have a child with a poor outcome.
Parental characteristics that may inhibit speech, including the way parents interact with the child. Parents need to follow a child’s lead and provide a language model using simplified speech. Use of “parentese,” the way that many parents instinctively talk to infants in a high-pitched, sing-song voice, actually fosters language development by attracting the infant’s attention and resembling the pitch of the sounds he makes.
Missed language explosion. Most children experience a vocabulary spurt around the age of 18 months, but late talkers don’t. Some late talkers have an “explosion” of speech later—between 24 and 30 months. If a child has not had a vocabulary spurt by 30 months, he is at considerable risk of continued language delay.
A primer on language and speech disorders Language disorders involve either receptive or expressive ability, or a combination of both. Receptive ability is the understanding of the spoken word—retrieving and processing sounds in the language storage centers of the brain and discriminating the differences between sounds in words, like cat versus pat. Expressive ability is how we learn to formulate grammatically and syntactically correct sentences.
A child with a receptive or expressive language disorder, or both, and no other developmental disability has specific language impairment (SLI), a condition also called language-learning impairment, developmental language disorder, developmental dysphasia, or developmental aphasia. In a recent study funded by the National Institutes of Health, the incidence of SLI in 5-year-olds was estimated to be 7.6%.7 Children with SLI are usually late talkers and most—67% to 84%—are boys.6 At 3 or 4 years old, most children with SLI have a limited vocabulary and speak in short phrases rather than sentences. If untreated, SLI can have an impact on school performance and career choices over the long term.4
The cause of SLI is unknown, but it appears to run in families. If a child has SLI, there is a 25% chance that another family member will be affected.
Speech disorders include disorders of articulation and phonology (dysarthria, apraxia, and phonologic disorder). Articulation refers to individual speech sounds and how they are pronounced. All children, not just those with a speech disorder, misarticulate sounds in the course of normal speech development. They may use sound substitutions such as “wady” for “lady”; omit sounds, saying “baw” instead of “ball”; or distort sounds, so that “snake” comes out “snek,” or “silly” comes out “shhilly.” Concern arises when these errors continue beyond the time a child normally outgrows them.
Phonologic development is the gradual process of acquiring adult speech. The majority of children pick up most phonologic rules by age 5. For example, most children stop deleting the final consonant in words (as when a child says “cuh” instead of “cup”) between ages 2 and 3. And children usually outgrow velar fronting by 3 years. An example of velar fronting is, “Mommy, tan you div me one?” (for “Mommy, can you give me one?”). In such cases, the child is replacing consonants made with the tongue moving toward the back of the mouth, such as “k” and “g,” with consonants produced at the front of the mouth: “t” and “d.”
Children with a phonologic disorder make sound substitutions consistently but, when given auditory and visual cues, are able to imitate correct sounds or words. Usually, they have normal oral muscle tone.
The dysarthrias are a group of motor speech disorders that result from nervous system injury. There is a lack of strength and control of the muscles used for both speech and non-speech functions, such as smiling and chewing. Many children with cerebral palsy have a dysarthric speech pattern, slurring words, distorting vowels, and often producing slow, labored, nasal speech. Many have an oral motor weakness, which probably first came to light as a feeding problem, accompanied by a protruding tongue, open mouth, or drooling. Dysarthria can also accompany other neurologic disorders, such as muscular dystrophy, myopathies, facial palsy, or closed head injury. Children with dysarthria have difficulty in the actual production of speech sounds. In particular, they are more likely to distort consonant sounds. This differs from apraxia, in which consonants are omitted.
Verbal apraxia is a neurologic motor speech impairment that affects the planning, executing, and sequencing of speech movements; that is, a breakdown in the neural transmission of messages to the muscles of the jaw, cheeks, lips, tongue, and palate. There is no obvious weakness in these muscles. To make themselves understood, these children may point, grunt, and become increasingly angry at their inability to communicate. Sometimes the same word can come out four different ways. The more these children try to talk, the more stymied they become and the harder they are to understand. They may drop the final consonant in single syllable words: “Cat come home” becomes “Ca co hoe.” They may transpose sounds within a word. Instead of saying “elephant,” they may say “efelant.” One day, an apraxic child says a difficult word perfectly—and then he loses it for weeks. He may also make unusual movements of his jaw, lips, and tongue, as if groping to find words. It’s obvious that he understands most of what is said to him, but he cannot respond properly. There is often a history of limited babbling and vocal play. The child may have an elaborate gestural communication system.
Some researchers have estimated that apraxia affects 6% to 10% of children.5 It can run in families and is often associated with neurologic soft signs. Many of these children have associated benign congenital hypotonia with low muscle tone in the trunk, affecting postural stability for respiration and phonation as well as motor coordination.8
What should take place during an office visit?
Children should receive the benefit of developmental surveillance and screening at each well visit. The American Academy of Pediatrics (AAP) has written policy statements emphasizing the need for developmental surveillance and screening from birth to 5 years old.9,10 The American Academy of Neurology (AAN) and Child Neurology Society (CNS), in a joint practice parameter on the screening and diagnosis of autism, also address early identification of language delays, as it is one of the early signs of a possible autistic spectrum disorder.11 These expert groups agree that parental concerns are usually well-founded and that pediatric practitioners should pay attention to them.
At every well visit, you should ask probing questions to determine whether your young patient has age-appropriate developmental skills (part of the process of developmental surveillance).12 Ideally, observe and assess the child’s developmental capabilities for yourself. This may seem like an almost impossible charge for a busy practitioner; parent questionnaires can help in this regard. Filled out beforehand at home or in the waiting room, they can be a valuable adjunct to your experience and clinical judgment and make the process more objective.
The Ages and Stages Questionnaire (ASQ) screens for developmental delay in infants from age 4 months to 5 years.13 Designed for use at every well visit, the ASQ is a series of questions covering each of five developmental domains: communication, gross motor, fine motor, problem solving, and personal-social. An additional section permits parents to express their concerns. For example, typical communication questions for 18-month-olds include, “When your child wants something, does she tell you by pointing to it?” and “Does your child say eight or more words in addition to ‘mama’ and ‘dada’?”
Another screening tool in parent questionnaire form, the Parents’ Evaluations of Developmental Status (PEDS), focuses specifically on the parents’ appraisal of areas of development.14 There is also the Denver II, which requires administration by the practitioner and can take about 20 minutes to administer—longer than most office visits.
 Whereas the ASQ and PEDS are parent-reporting screening instruments that can be used for general developmental screening, the Checklist for Autism in Toddlers (CHAT) can be used to screen specifically for autism from 18 to 36 months of age.15 There are nine yes-no questions answered by the parent and five brief interactions between the child and the practitioner. It takes only five to 10 minutes to administer and score, and it can be downloaded from the Web without charge ( http://www.nas.org.uk ; search for “CHAT”).
Whereas the ASQ and PEDS are parent-reporting screening instruments that can be used for general developmental screening, the Checklist for Autism in Toddlers (CHAT) can be used to screen specifically for autism from 18 to 36 months of age.15 There are nine yes-no questions answered by the parent and five brief interactions between the child and the practitioner. It takes only five to 10 minutes to administer and score, and it can be downloaded from the Web without charge ( http://www.nas.org.uk ; search for “CHAT”).
Whichever tool(s) you use, the bottom line is this: You should conduct routine developmental surveillance at every well-child visit, as called for in the practice parameter algorithm put forth by the AAN/CNS for screening and diagnosis of language delays and children specifically at risk of autism.10 Absolute indications for immediate evaluation (Table 3) are11:
no babbling, pointing, or gesturing by 12 months
no single words by 16 months
no two-word spontaneous phrases by 24 months
any regression in language or social skills at any age
Any child with a delay in language or social development should have a formal hearing evaluation by an audiologist, even if he had a hearing screening at birth. This is especially critical in the child who has a history of otitis media with effusion, in which case referral to a pediatric otolaryngologist may also be warranted.
A lead screening is an especially important laboratory investigation in a child with developmental delay. Some of these children spend a prolonged time in the oral-motor stage of play15 and are at risk of lead toxicity. An elevated lead level can cause behaviors that resemble developmental delay, autism, and emotional disturbance.11
When and where to refer If hearing is within normal limits and a child fails a developmental screening (ASQ, PEDS, CHAT) or has an absolute indicator for immediate evaluation, referral to a professional who can perform a comprehensive developmental evaluation is in order. It is advisable to consult a developmental-behavioral pediatrician, pediatric neurologist, or child psychologist if a diagnosis of autism or a disorder of neurologic etiology is suspected. A neurodevelopmental physician is recommended if a laboratory work-up or neuroimaging is indicated. If you do not believe that a full neurologic work-up is indicated, referral to a private speech-language pathologist for evaluation of a speech or language delay is appropriate. Referral to a child psychiatrist may be appropriate if there are coexisting psychiatric problems. (A “letter of medical necessity “from a physician is often helpful to parents when they are seeking health insurance reimbursement for private evaluations or therapy.)
If the child is an infant or toddler, you should simultaneously refer him, with parental consent, to the local early intervention (EI) program, where he will receive a multidisciplinary evaluation to determine his eligibility for habilitative services. If he’s older than 3, refer him to the local school district for a developmental evaluation to see if he qualifies for special services.
 There are also many activities parents can do at home with their child to promote the development of speech.
There are also many activities parents can do at home with their child to promote the development of speech.
These are detailed in the Guide for Parents -This guide was written by Lisa Geng. Ms. Geng is co-author of The Late Talker What to Do If Your Child Isn’t Talking Yet.
The Individuals with Disabilities Education Act (IDEA)16 requires that EI services be provided for children from birth through age 3. Any child suspected of having a delay in any aspect of his development is entitled to an evaluation to see if he is entitled to interventional services. To be eligible, children must either have a diagnosed condition with a high probability of developmental delay (such as Down syndrome or meningomyelocele) or an established delay in physical, cognitive, communication, social-emotional, or adaptive (self-help) development. For the purposes of EI, a developmental delay is documented as a 33% delay in one area of development or a 25% delay in each of two areas. For example, a 24-month-old would qualify for services if he is functioning at the 16-month level in communication ability or at an 18-month level in both communication and physical (motor) areas.
EI, also known as the Birth to Three Program, is a family-centered program. Parental consent is required for an evaluation, and parents participate in establishing goals and monitoring outcomes. In some states, the program is free; in others, there is a sliding scale of costs depending on the parents’ income. EI services are usually provided in “natural environments, “which may be the child’s home, the day-care center, or the playground. Services vary from state-to-state, but the evaluation is usually conducted in the family’s home.13
Regrettably, many children with speech and language disorders are not afforded the opportunity to benefit from EI because they are not referred into the program before their third birthday. To avoid this, it is advisable to discuss this program with the family of a child who has signs of a communication delay, even if you believe that the child might “outgrow” his delay. Parents may also choose to self-refer. If your office does not have the contact information for referral to EI, your state’s EI official designee can be located through the National Early Childhood Technical Assistance Center (NECTAC), http://www.nectac.org/, or the local department of health.
After 3 years of age, IDEA guarantees a “free and appropriate public education ” (FAPE) to every child through 21 years old in need of special education services. Public schools must provide services in the “least restrictive environment,” and must create and implement an individualized education program (IEP) specifically designed to meet each child’s needs. In addition to the special educational component, the IEP must include “related services” such as speech, physical, and occupational therapies. It also covers the provision of transportation, augmentative communication devices, and counseling services.17
What’s at stake A child who demonstrates communication delay as a toddler and during preschool is at greater risk of later language-based learning disabilities, including reading disabilities (dyslexia). These children typically have deficits in phonologic awareness, the ability to segment words into sounds, and expressive language disorders.18
Communication problems can also be damaging to a child’s social life. “Even if a delay is transitory,” states a report from New York State’s Early Intervention program, “a communication delay at a young age may have an impact on the child’s ability to form relationships with peers and adults and, therefore, may impact the child’s overall development.”19 Because many children with a speech disorder do not know the rules of conversation and social interaction, their behavior can become inappropriate (hitting another child, for instance, to let him know he wants to play) and harm their chances of making and maintaining friends. Social failure atop academic failure can lower self-esteem.
Rice and colleagues found that children with communication impairments were frequently ignored by other kids and were not as popular as so-called typically developing classmates. This bias was commonly shared by adults, including teachers and speech-language pathologists. Rice also found that adults consistently rate children with communication impairments as less intelligent and less socially competent than their peers.
In a 14-year study at the University of Toronto, 240 5-year-old youngsters with speech and/or language impairment were followed to assess the “psychiatric outcome” of growing up with a language impairment. At the age of 19, the group had a statistically signifiher incidence of anxiety and antisocial personality disorders.22
 Recognizing the developmental and educational gains for the child, the family, and society, the US DOE has endorsed early intervention, noting that EI services have resulted in children needing fewer special education and other services later in life and being retained in a grade less often.23 EI also has a cost-saving benefit, according to the National Early Childhood Technical Assistance Center. In one study, 3- and 4-year-olds from a poor family were followed up shortly after their expected date of high school graduation. The children who had received EI had required less special education, were more likely to graduate, and were less likely to get into trouble with the law. Based on projected lifetime earnings and other assumptions, the analysts assessed that early intervention returned $3 for every $1 invested.24
Recognizing the developmental and educational gains for the child, the family, and society, the US DOE has endorsed early intervention, noting that EI services have resulted in children needing fewer special education and other services later in life and being retained in a grade less often.23 EI also has a cost-saving benefit, according to the National Early Childhood Technical Assistance Center. In one study, 3- and 4-year-olds from a poor family were followed up shortly after their expected date of high school graduation. The children who had received EI had required less special education, were more likely to graduate, and were less likely to get into trouble with the law. Based on projected lifetime earnings and other assumptions, the analysts assessed that early intervention returned $3 for every $1 invested.24
Erring on the side of caution Your primary care role in early identification of children with a developmental delay has been underscored in policy statements from the Committee on Children with Disabilities of the AAP several times over. You are asked to provide a medical home for children and families who may have a developmental delay or a special health-care need, and you are in a position to be the “first point of contact when parents have concerns about their child’s development or behavior.”25 When these concerns are ignored or dismissed, parents often become frustrated and angry, especially if the child is diagnosed with an autistic spectrum disorder, apraxia, or language impairment a year or more after symptoms were recognized.
The notion that all late talkers are “little Einsteins” is a myth; not all these children have a positive outcome with a wait-and-see approach. Reviewing the “Predictors of continued language delay” should help guide you in deciding whom to refer for further evaluation. If you are unsure whether a child is presenting with just a delay, don’t gamble! Refer the family to a developmental specialist for an expert’s opinion.
Of course, not every child evaluated needs intervention; most who present as a late talker develop normally. But if the child is later found to have had a delay in maturation and not a disorder, what’s the downside of having intervened? Not much. Some time and, perhaps, some expense on the part of the parents or their health-care insurer. And the upside? Relieved parents who are both confident that their child’s language development is age-appropriate and grateful that you have taken such an interest in their child’s development and not just in his physical health.26
Marilyn C. Agin, MD is on the medical staff of the department of pediatrics, section of developmental pediatrics, St. Vincent’s Hospital and Medical Center, New York, N.Y. She is medical director of New York City Early Intervention Program and is in private practice in NYC. Along with Lisa Geng, she is co-author of The Late Talker — What to Do If Your Child Isn’t Talking Yet (St. Martin’s Press, 2003). Dr. Agin has nothing to disclose in regard to affiliations with, or financial interests in, any organization that may have an interest in any part of this article.
REFERENCES
1. US Department of Education: Number of Children Served under IDEA, Part B by Disability and Age, During the 1999-2000 School Year (table), in Twenty-third Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act, 2001; http://www.ed.gov/about/reports/annual/osep/2001/index.html
2. Glascoe FP: Communicating with parents. Young Exceptional Children 1999;2(4):16
3. New York State Department of Health Early Intervention Program data, 7/98-7/99, (internal records) Albany, N.Y.
4. New York State Department of Health, Early Intervention Program. Clinical Practice Guideline: The Guideline Technical Report, Communication Disorders, Assessment and Intervention for Young Children (Age 0-3 Years). 1999, New York State Department of Health, Albany, N.Y.; II 3-16, III 13-25, III 85, III 89-95
5. Agin MC, Geng LF, Nicholl MJ: The Late Talker, What to Do If Your Child Isn’t Talking Yet. New York, N.Y., St. Martin’s Press, 2003
6. Olswang LB, Rodriguez B, Timler G: Clinical Focus. Recommending intervention for toddlers with specific language learning difficulties. Am J Speech Lang Pathol 1998;7(1):23
7. Ervin M: SLI: What we know and why it matters. The AHSA Leader online. http://www.asha.org/about/publications/leader-online/archives/2001/sli.htm
8. von Raffler-Engel W, Wind J, Jonker A (eds): Studies in Language Origins, Volume 2. Amsterdam/Philadelphia, John Benjamins Publishing Co., 1991, pp 123-157
9. Committee on Children with Disabilities of the American Academy of Pediatrics: Screening Infants and Young Children for Developmental Disabilities. Pediatrics 1994;3:863
10. Committee on Children with Disabilities of the American Academy of Pediatrics: Developmental Surveillance and Screening of Infants and Young Children. Pediatrics 2001;108:192
11. Filipek PA, Accardo PJ, Ashwal S, et al: Practice parameter: Screening and diagnosis of autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000;55:468
12. Dworkin P: Developmental screening: (Still) expecting the impossible? Pediatrics 1992;89:1253
13. Agin M, Huberman H, Lobach K: Developmental delay in young children. City Health Information (CHI) 2001;20(3):1
14. Glascoe FP: The Parents’ Evaluations of Developmental Status (PEDS): A method for detecting and addressing developmental and behavioral problems in children. Accessed at http://www.pedstest.com/
15. Baron-Cohen S, Allen J, Gillberg C: Can autism be detected at 18 months? The needle, the haystack, and the CHAT. Br J Psychiatry 1996;168:158
16. US Government: 99th Congress. Public Law 99-457
17. US Department of Education: Selected OSEP memoranda and other publications regarding IDEA, http://www.ed.gov/policy/speced/guid/idea/omip.html
18. Shaywitz SE: Dyslexia. N Engl J Med 1998;338:307
19. New York State Department of Health, Early Intervention Program: Clinical practice guideline: The guideline technical report, communication disorders, assessment and intervention for young children (age 0-3 years). 1999, New York State Department of Health, Albany, N.Y.; II-10
20. Rice M, Sell M, Hadley P: Social interactions of speech-and-language-impaired children Journal of Speech and Hearing Research 1991;34:1299
21. Rice ML: “Don’t Talk to Him; He’s Weird”: A social consequences account of language and social interactions, in Enhancing Children’s Communication: Research Foundations for Intervention, Kaiser AP, Gray DB (eds), Baltimore, Md., Brookes Publishing Co, 1993
22. Beitchman JH, Wilson B, Johnson CJ, et al: Fourteen-year follow-up of speech/language-impaired and control children: Psychiatric outcome. J Am Acad Child Adolesc Psychiatry 2001;40(1):75
23. US Department of Education: The 22nd Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act, 2000
24. National Early Childhood TA Center: Economic Impact Studies, http://www.nectac.org/topics/effective/economic.asp
25. Committee on Children with Disabilities of the American Academy of Pediatrics: The pediatrician’s role in the diagnosis and management of autistic spectrum disorder in children. Pediatrics 2001;107:1221
26. Kaminer R, Jedrysek E: Early identification of developmental disabilities. Ped Annals 1982;11:427

A whole lot of good info here that I wish I had many moons ago
Thanks Vickie!